Training plans are currently available for the following diagnoses:
Flat back
The natural curvature of the spine is only slightly pronounced in a flat back. The pelvis is strongly upright and the posture is unusually straight. Due to the below-average S-curvature, the spine lacks its natural shock absorber function, which means that the effects on the intervertebral discs must be compensated for.
The unfavorable pressure distribution can cause severe back pain when under strain, as the intervertebral discs and joints wear out quickly. In addition to severe wear and tear, the supply of nutrients is also restricted as a result of the high pressure on the lower vertebrae. If a flat back is not treated, it can also lead to restricted mobility and poor performance, which is associated with a deterioration in quality of life.
A flat back can be a symptom of another underlying disease, but it can also be caused by posture problems. Poor posture often develops in childhood. If this posture is maintained during the growth phase, the spine will develop in line with this posture, which can lead to misalignment and pain.
First, it is important to identify the cause of the flat back. In most cases, conservative treatment is promising. Targeted stretching and strengthening exercises as well as activation of the core muscles are intended to improve posture and create muscular balance. Shortened muscles are stretched and weakened muscles are strengthened in order to eliminate muscular imbalances and distribute the load evenly across the musculoskeletal system.
The training is designed to help your spine regain its natural S-shape. So make sure you maintain the correct spinal posture while performing the exercises. Your cervical and lumbar spine should be aligned forward, while your thoracic spine and sacrum should be aligned backward.
If you feel pain during the exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
Buchbauer J. Präventives Muskeltraining zur Behebung von Haltungsfehlern: Totalrundrücken, Hohlrücken, Hohlrundrücken, Flachrücken und Skoliose; Gymnastik – Gerätetraining – Ernährung. Schorndorf: Hofmann; 1999.
Hyperkyphosis (hunchback)
Hyperkyphosis is a deformity of the spine that causes the upper back to curve forward. While kyphosis (curvature outward) in the thoracic spine is normal, hyperkyphosis causes this curvature to become so severe that it is no longer within the normal range. When viewed from the side, hyperkyphosis is characterized by a rounded back. The head and neck are positioned in front of the torso.
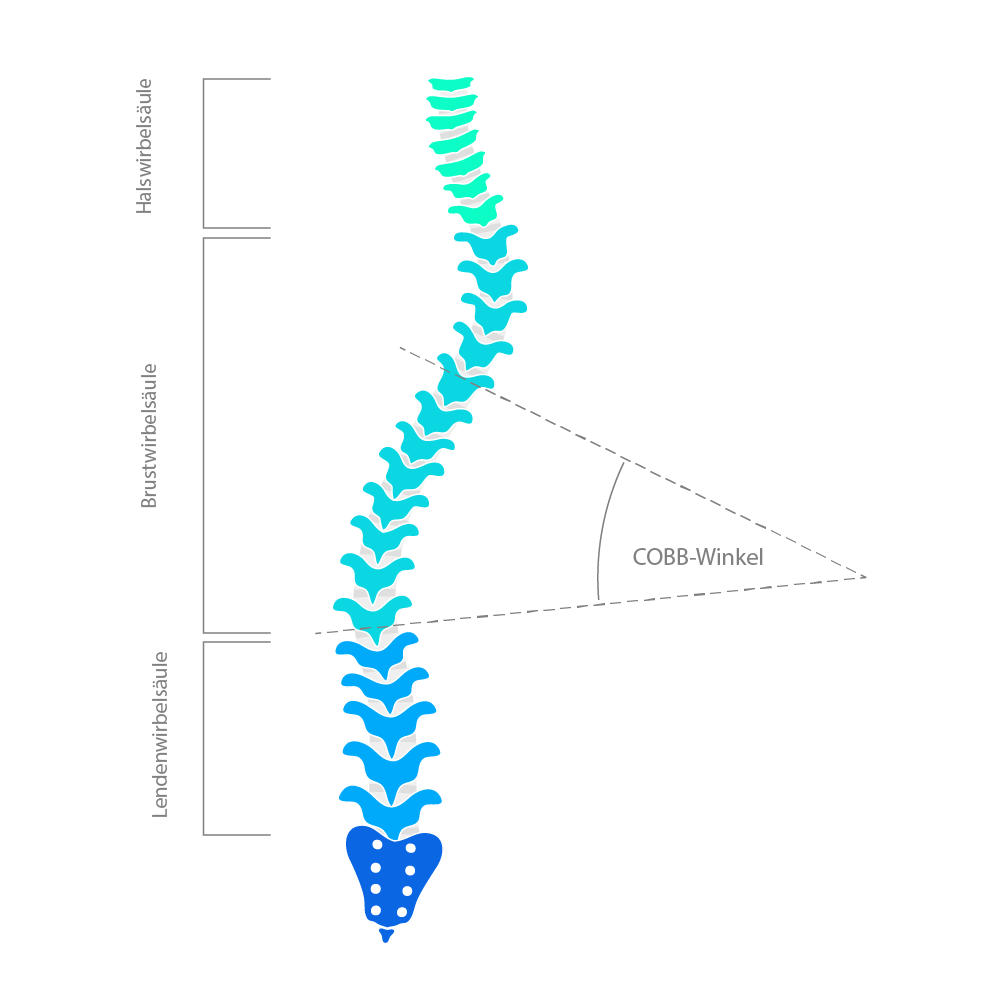
Similar to scoliosis, the extent of hyperkyphosis is calculated using the Cobb angle.
When determining the cause of this condition, a distinction must be made between congenital and acquired hyperkyphosis. In congenital hyperkyphosis, the problems are present from birth and are referred to as congenital hyperkyphosis.
The acquired form is much more common. In this case, there are many different causes that can lead to the development of a hunched back. These include poor posture, lack of exercise, and associated muscle weakness. Prolonged sitting causes the thoracic spine to fall forward, and because the shoulder and back muscles are too weak, the imbalance cannot be counteracted—the muscular imbalance becomes entrenched.
In addition, various diseases can cause hyperkyphosis. Degenerative disc disease, osteoporosis, or Scheuermann’s disease (abnormal ossification of the thoracic spine) are possible causes.
Hyperkyphosis can be treated effectively with targeted training. Exercises that help to straighten the body, specific stretches, and muscle strengthening can reduce the curvature of the spine and alleviate pain.
In addition, special breathing exercises help to relieve the muscles and allow the lungs to expand again. This can also prevent the condition from progressing.
To correct hyperkyphosis, it is very important to perform the recommended exercises regularly. However, if you feel pain during an exercise or if the pain becomes more severe, stop the exercise and indicate this in the app’s feedback function.
You should also pay attention to maintaining a healthy posture in everyday life. Avoid repetitive movements and heavy lifting, and make sure you get enough exercise.
Rusu, C., Herold, L., Voigt, C. et al. Thorakolumbaler Übergang der Wirbelsäule. Trauma Berufskrankheiten. Volume 9, S249–S256 (2007).
Katzman, W.B., Wanek, L., Shepard, J.A.; Sellmeyer, D.E. . Age-Related Hyperkyphosis: Its Causes, Consequences, and Management. Journal of Orthopaedic & Sports Physical Therapy. Volume40, Issue6, Pages 352-360 (2010).
Hyperlordosis (hollow back)
Hyperlordosis is an unusually strong forward curvature of the spine. It most commonly occurs in the lumbar spine and is known as a “hollow back.” The pelvis and abdomen are extremely arched forward, and the chest shifts backward to compensate.
The most common cause of hyperlordosis is poor posture combined with too little exercise. Sitting for long periods of time often shortens the back muscles and increases the tension on the muscles and fascia. In addition, weak back and abdominal muscles promote the development of hyperlordosis. Severe obesity and the associated postural changes or osteoporosis are further risk factors.
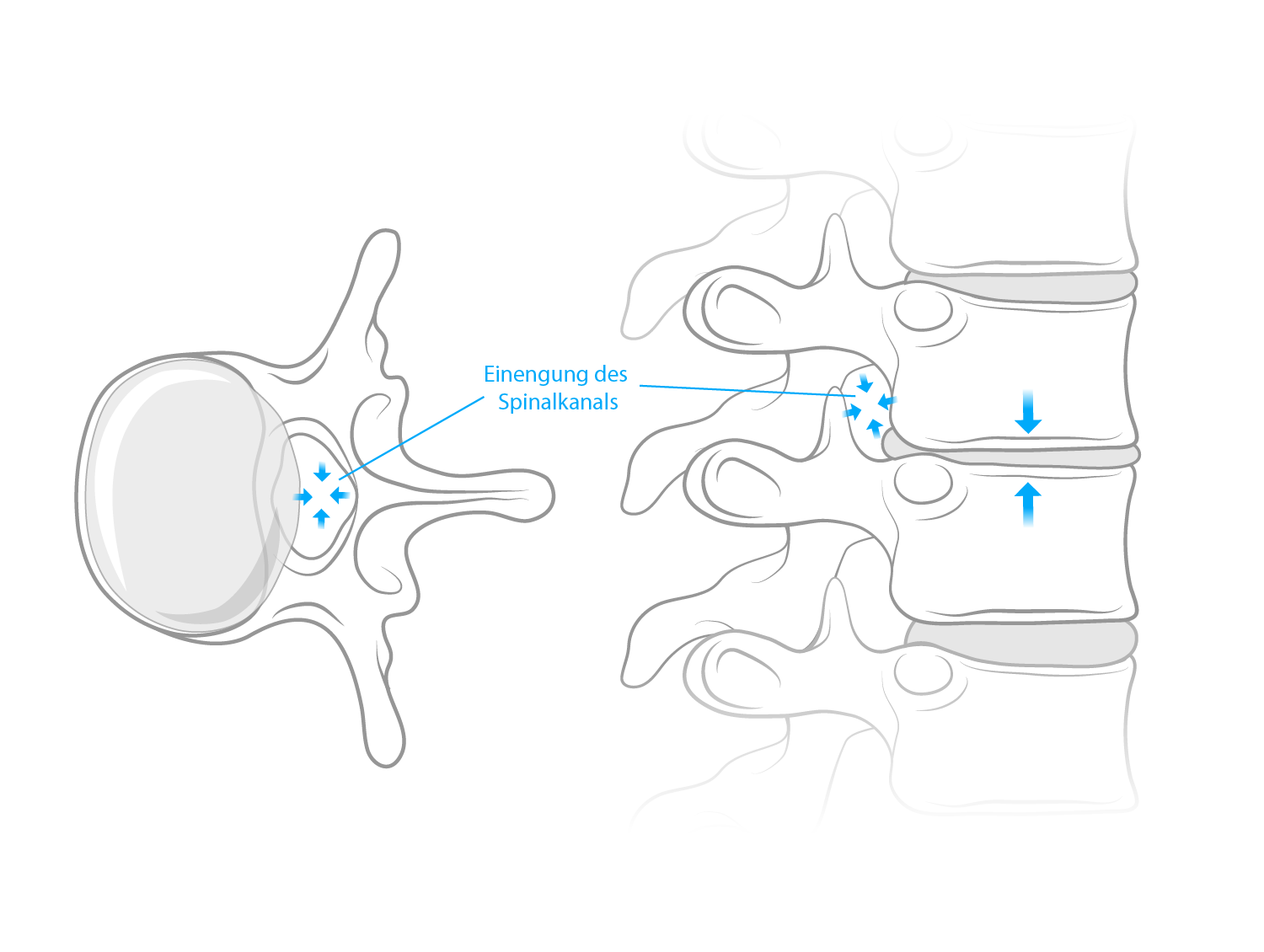
If hyperlordosis is left untreated, it can have various consequences. As the intervertebral discs are subjected to heavy strain, this can lead to a slipped disc in extreme cases. Narrowing of the spinal canal is also a possibility.
However, hyperlordosis can be managed well with special exercises. The aim is to correct muscular imbalances. The back extensors and hip flexors are usually tense, while the abdominal and gluteal muscles are too weak. Selected stretching and strengthening exercises can help you relearn the correct posture. However, this is a lengthy process that involves integrating movement into your everyday life, dynamic sitting, and controlling your own posture.
Certain relaxation techniques can also be part of the therapy to loosen tense muscles.
When performing the exercises, make sure to keep your stomach tense and actively work against the hollow back position. You should check your back posture regularly and pay attention to your posture. Your shoulders should fall loosely back, and your buttocks and stomach should be tense.
If you feel pain during an exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
Sadler SG, Spink MJ, Ho A, De Jonge XJ, Chuter VH. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: a systematic review of prospective cohort studies. BMC Musculoskelet Disord. 2017;18(1):179. Published 2017 May 5. doi:10.1186/s12891-017-1534-0
Brötz, D., Weller, M. (2017). Diagnostik und Therapie bei Bandscheibenschäden, 4. Auflge
Disc protrusion
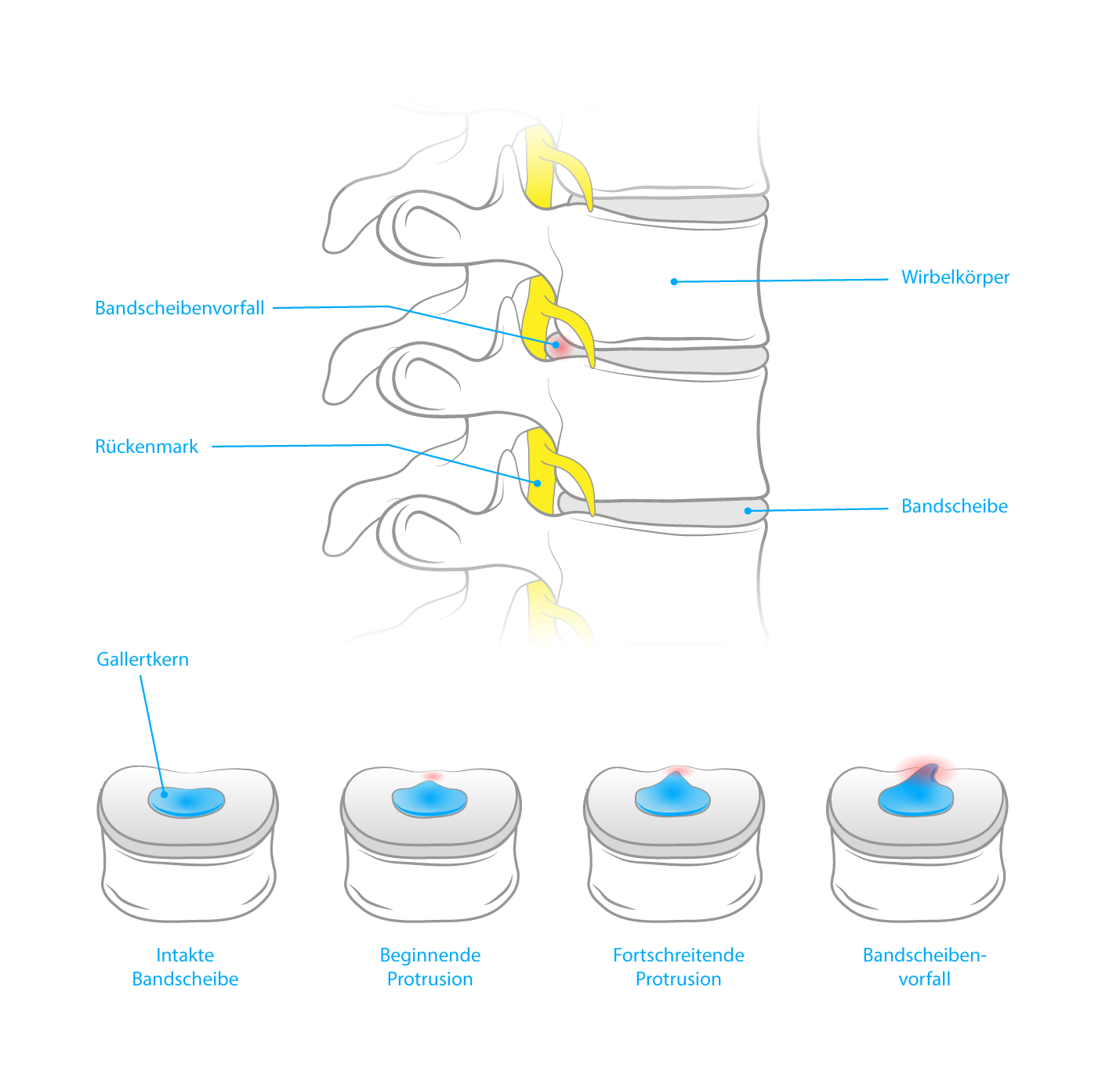
A disc protrusion describes a forward bulging of the fibrous ring of the intervertebral disc and is thus the precursor to a herniated disc (disc prolapse). In contrast to a herniated disc, however, there is no tear in the fibrous ring, but only a bulge caused by the inner gelatinous core expanding to the side.
Such bulging can occur in any section of the spine, but is most common in the lumbar spine.
There are many causes of disc protrusion. Degenerative changes contribute significantly to the development of disc protrusion. The water retention capacity of the gelatinous core decreases with age, causing the tissue of the outer fibrous ring to become porous. This increases the risk of protrusion when under strain, for example when lifting heavy loads.
Heavy physical work, poor posture, traumatic injuries, lack of exercise, and obesity increase this risk.
Regardless of age, such protrusion can be caused by high forces in an accident or by a congenital weakness of the connective tissue.
Targeted strengthening of the surrounding muscles is the most important aspect of treating a disc protrusion. In general, care should be taken to train all the supporting muscles in the torso in order to stabilize the spine as much as possible and prevent the protrusion from progressing further.
Back training and the correction of possible poor posture are also part of conservative treatment.
If you feel pain during an exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
To prevent further disc protrusions, you should continue to strengthen your back and stabilize your spine even after the pain has subsided. Also, make sure you lift and carry things correctly in everyday life to relieve strain on your back.
Wottke D. (2004) Orthopädie. Die große orthopädische Rückenschule. Springer, Berlin, Heidelberg.
Streeck U., Focke J., Melzer C., Streeck J. (2017) Manuelle Therapie und Rehabilitation der Lendenwirbelsäule. In: Manuelle Therapie und komplexe Rehabilitation. Springer, Berlin, Heidelberg.
Skoliosis
Scoliosis refers to a lateral deviation or curvature of the spine accompanied by twisting.
A distinction is made between idiopathic scoliosis (the most common form, accounting for approximately 85% of cases) and symptomatic or secondary scoliosis.
There is no specific cause for the development of idiopathic scoliosis. However, it can be attributed to uneven growth of the back muscles and vertebrae. This form of scoliosis occurs mainly during periods of rapid growth, which is why children and adolescents are particularly affected.
If scoliosis is attributable to another diagnosis, it is referred to as symptomatic scoliosis. This can be caused, for example, by a disease of the nervous system, a disease of the muscles, or bone metabolism.
The Cobb angle can be used to indicate the severity of the lateral curvature of the spine. A curvature of the spine of 10 degrees or more is referred to as mild scoliosis. If the angle is between 40 and 60 degrees, it is considered moderate scoliosis, and if it is over 60 degrees, it is considered severe scoliosis.
Depending on which side the spine curves to, it is referred to as left- or right-convex scoliosis.
The good news is that mild scoliosis can be treated with simple therapeutic exercises, which can counteract further curvature. The aim is to strengthen the back muscles and correct posture as much as possible.
Avoid jerky and sudden movements that put too much strain on the spine. Make sure you perform the exercises in a controlled and stable manner and keep your spine straight. To increase the tension, gently pull your navel inwards during the exercises.
If you feel pain during the exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
Radl, R., Maafe, M. & Ziegler, S. Skoliose. Orthopäde 40, 449–462 (2011). https://doi.org/10.1007/s00132-011-1771-0
Lumbar spinal stenosis
The spinal cord runs through a canal (spinal canal) in the spine. If this canal is narrowed, this is referred to as stenosis. If, as in most cases, this narrowing occurs at the level of the lumbar spine, it is referred to as lumbar stenosis or lumbar spinal canal stenosis. The pressure on the spinal cord and blood vessels caused by the narrowing manifests itself in the form of back pain that radiates into the legs.
In most cases, age-related wear and tear of the spine is the cause. The height of the intervertebral discs decreases, as does the distance between the vertebral bodies. This leads to a protrusion of the intervertebral disc into the spinal canal and reduced elasticity of the ligaments along the spine. The spinal canal becomes further narrowed and the entire spinal segment becomes unstable.
Other causes include the development of osteoarthritis of the vertebral joints, as bony growths on the vertebral bodies can narrow the spinal canal, congenital malformations, or bone diseases.
Idiopathic spinal canal stenosis describes the narrowing of the spinal canal from birth for unknown reasons.
The main goal of therapeutic training for stenosis is to relieve pressure on the spine. Particular attention should be paid to choosing exercises that reduce the hollow back position (lordosis) of the lumbar spine. These include stretching exercises for the hip flexors and front thigh muscles, as well as strengthening exercises for the abdominal muscles. Back-friendly postures should be taught and general stabilization and targeted strengthening of the back muscles should be achieved.
When performing the exercises, make sure you do not fall into a hollow back position and keep your abdomen tense. To intensify the tension, gently pull your navel toward your spine.
If you feel pain during the exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
Jeanneret, B., Jeanneret, C., Der enge Spinalkanal der LWS. Swiss Med Forum. 2002; 02(39), S.922-928
Bodack MP, Monteiro M. Therapeutic exercise in the treatment of patients with lumbar spinal stenosis. Clin Orthop Relat Res. 2001;(384):144-152. doi:10.1097/00003086-200103000-00017
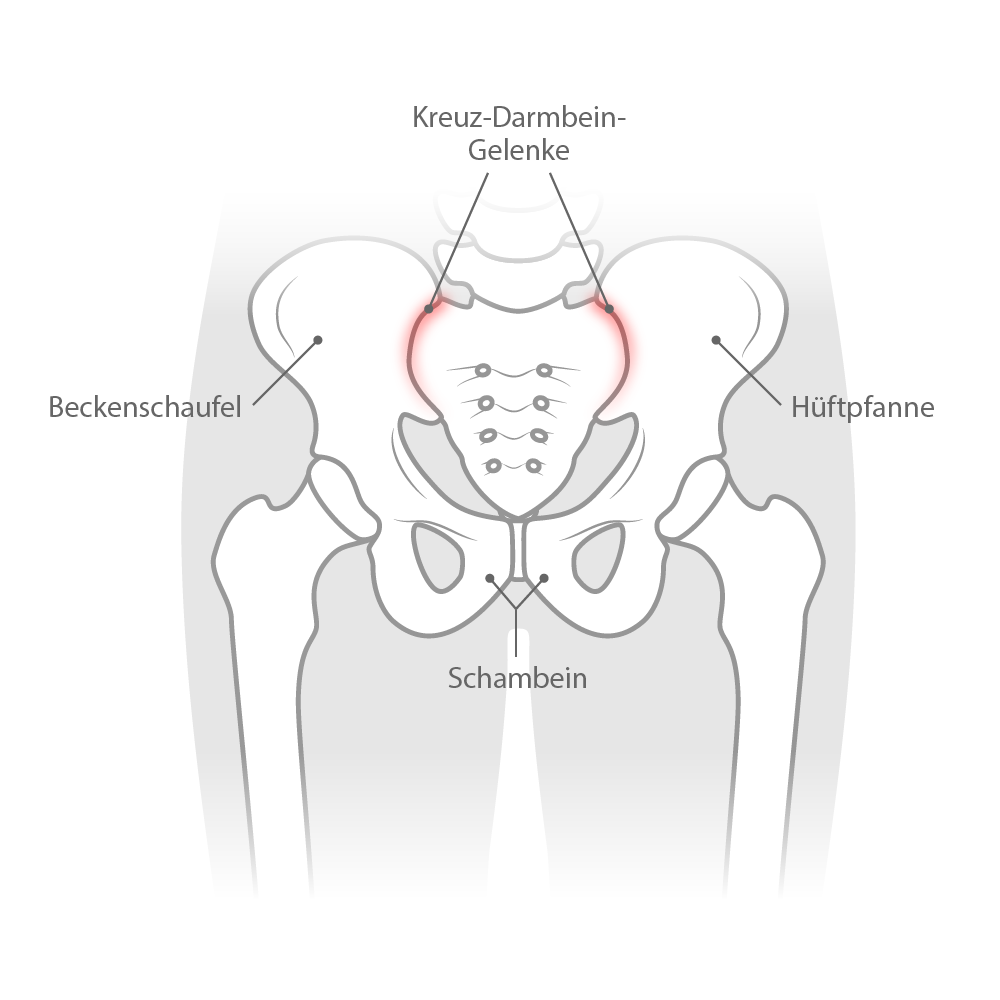
SI joint blockage
SI joint dysfunction describes a dysfunction of the sacroiliac joint. The joint’s mobility is restricted due to the joint surfaces of the sacrum and ilium becoming misaligned, which can lead to pain in the lower back that radiates to the buttocks and the rear thigh muscles. If the symptoms occur over a longer period of time, this is referred to as SI joint syndrome.
There are many causes of SI joint dysfunction. Poor posture, heavy lifting, or being overweight are the most common triggers. Sudden stopping movements or stepping into thin air, such as when missing a step on the stairs, can also cause SI joint dysfunction.
In addition, hormonal changes during pregnancy cause the ligaments to loosen. Combined with increased weight, this leads to a loss of stability, muscle tension, and joint blockage.
In most cases, SI joint blockage can be treated effectively with conservative therapy. The aim is to mobilize and relieve the SI joint area through specific stretching and strengthening exercises. In addition, the back and abdominal muscles should be strengthened to stabilize the upper body.
Normal movement patterns should be regained as quickly as possible to prevent the pain from becoming chronic.
In addition to the recommended mobilization and strengthening exercises, it is very important to get enough exercise despite the pain when suffering from an SI joint blockage.
However, if the pain becomes more severe during the exercise, stop the exercise and indicate this in the app’s feedback function.
Even after the blockage has been resolved, care should continue to be taken to strengthen the surrounding muscles and stabilize the lumbar-pelvic region as much as possible. This significantly reduces the risk of recurrence.
Schenker, A., Schiltenwolf, M., Schwarze, M. et al. Schmerzquelle Iliosakralgelenk. Orthopäde (2019). https://doi.org/10.1007/s00132-019-03843-1
Mohadjer, S. Diagnose und Therapie des “Iliosakralgelenksyndroms” – Eine gesundheitliche, psychosoziale und schmerzrelevante Betrachtung (2008). URN: urn:nbn:de:bsz:25-opus-60926
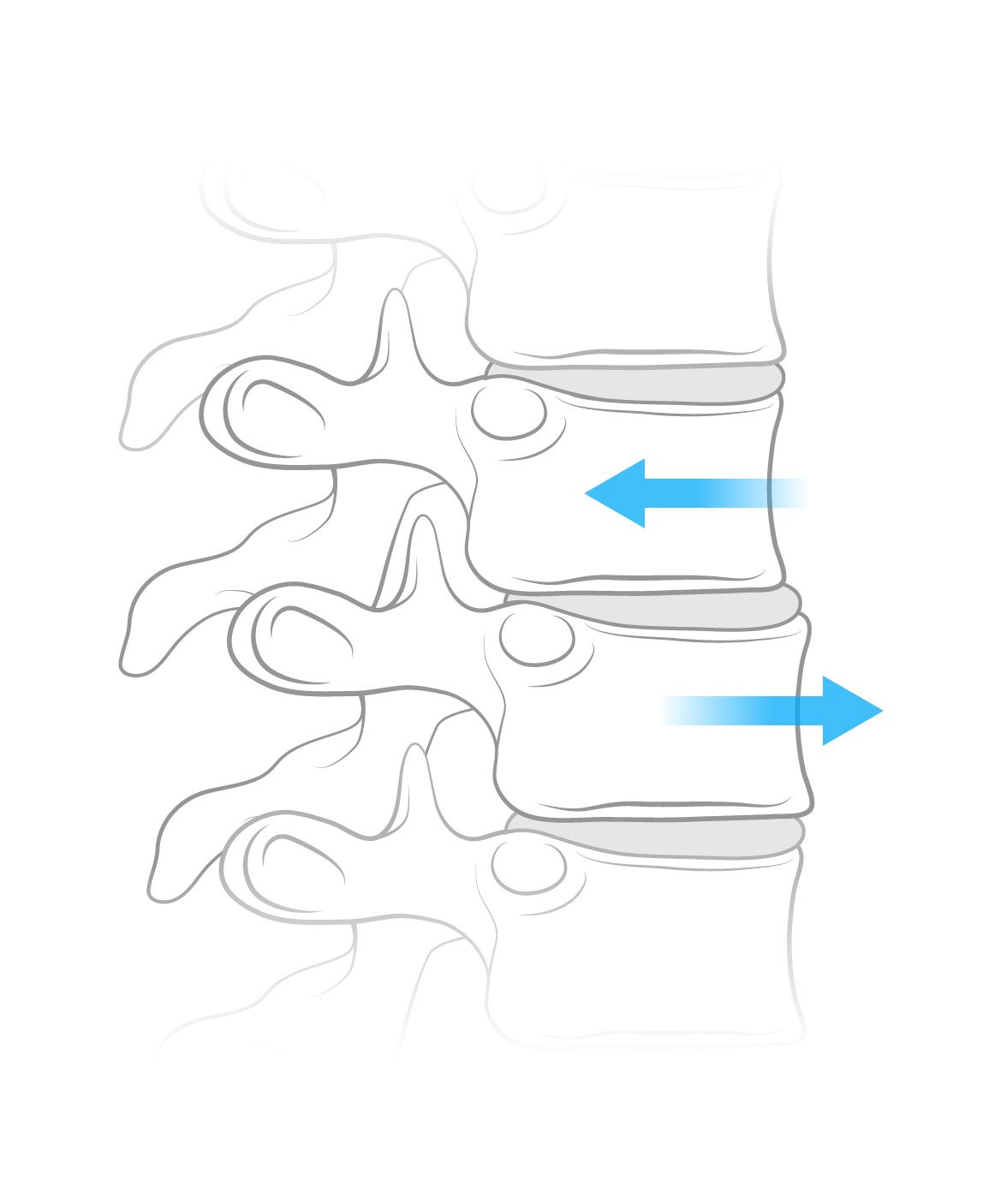
Spondylolisthesis
If a vertebral body leaves its original position in the spine and shifts due to instability, this is referred to as spondylolisthesis. If the vertebra shifts forward in relation to the others, this is referred to as ventral spondylolisthesis; if the vertebra shifts backward, this is referred to as dorsal spondylolisthesis. The lumbar spine is most commonly affected.
The most common cause of spondylolisthesis is wear-related (degenerative) damage to the spine. Age-related fluid loss in the intervertebral discs causes them to lose height. As a result, the vertebral bodies move closer together, which disrupts the function of the musculoskeletal system. Another cause is the formation of a gap in the vertebral arch. If this section of bone is damaged, the vertebra becomes more mobile and can slip out of the spinal axis.
Bone loss, previous fractures, and congenital deformities of the spine can also be cited as reasons for the development of a slipped vertebra.
Strengthening the lumbar spine is a central component of conservative therapy for spondylolisthesis. In addition to general stabilization of the spine, particular attention should be paid to the back extensors and abdominal muscles.
Surgery is only considered when neurological deficits become apparent as a result of the spondylolisthesis.
Avoid jerky and sudden movements that put too much strain on the spine. In addition, frequent hollow back positions and twisting movements can promote spondylolisthesis in the long term.
If you feel pain during the exercise or if the pain gets worse, stop the exercise and indicate this in the app’s feedback function.
R. Krämer et al., Die lumbale Spinalkanalstenose, DOI 10.1007/978-3-642-13843-0_6,© Springer-Verlag Berlin Heidelberg 2012