A detailed medical history is particularly important for back pain due to its diverse manifestations.
The distinction between “red flags” and “yellow flags” plays an important role here. The “red flags” are warning signs of specific causes for the back pain that require immediate clarification of the therapy. These include strong signs of inflammation, unclear fever or neurological deficits. The “yellow flags” indicate psychological risk factors that can lead to back pain becoming chronic. Chronicity occurs when acute pain develops into a permanent problem (> 12 weeks).
Development of chronic back pain
Back pain is one of the most common chronic pain symptoms today. A variety of psychosomatic and psychobiological mechanisms are highly relevant to the development of chronic back pain. Stress at work, in private life or unprocessed events are potential triggers. The reason for this is increased muscle tension, which is caused by increased alertness.
The fear of aggravating the pain starts the vicious circle. Movements are avoided, a protective posture is adopted and self-confidence is weakened. Due to the so-called pain memory, the brain can perceive pain as a long-term consequence, even though there are no longer any acute stimuli.
The close relationship between physical and psychological processes can be summarised under Engel’s bio-psycho-social pain model. According to this model, pain is a multidimensional syndrome that has an impact on three levels (see graphic).
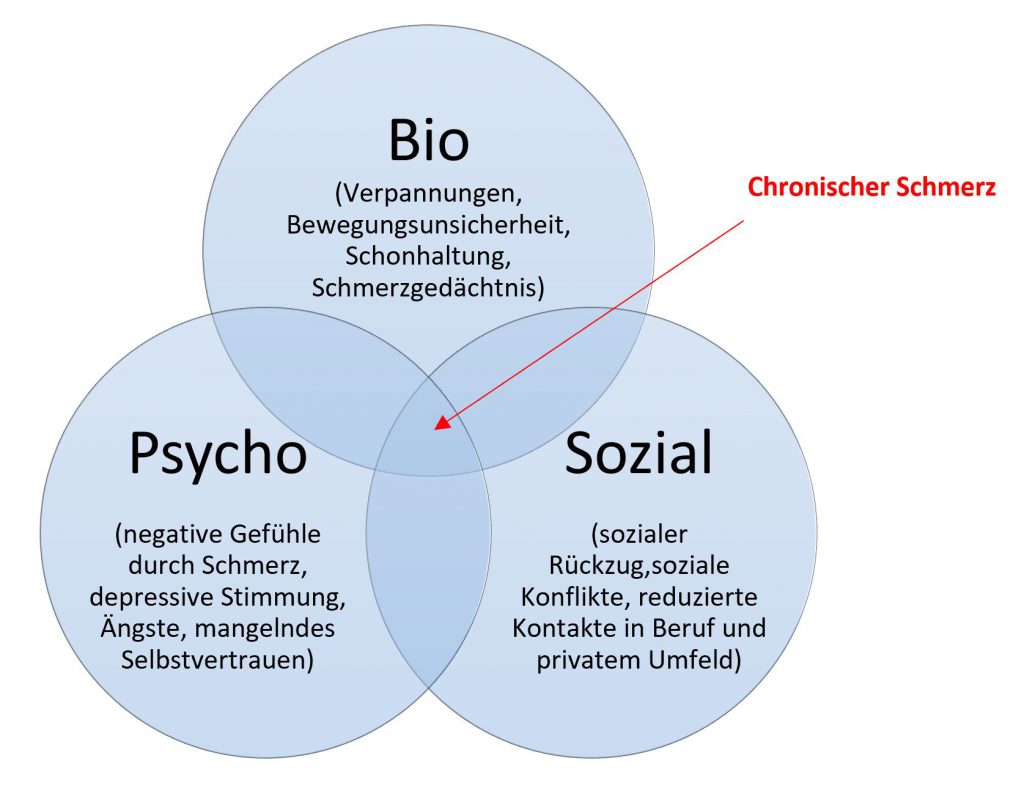
Bio-psycho-social pain model according to Engel
Everyday tasks often mean new challenges as a result of the pain, which causes people to question their own competences and role function. Psychological aspects, such as self-image, have to be adapted to the new situation. In an attempt to avoid the pain and the reduced ability to perform, people withdraw socially, which often leads to psychological isolation. Concomitant mental illnesses such as depression are possible consequences.
Treatment of chronic back pain
Therapeutic approaches that integrate the psychological and social aspects of chronic pain are of great importance in treatment. Back pain should always be considered in terms of its complex interactions and different levels, as symptom relief alone is often not sufficient. In order to prevent the pain from becoming chronic again once it has been relieved, emphasis should also be placed on regular physical activity and continued monitoring of the patient’s psychosocial structures.
Sources:
• Baron et al. (2013); Praktische Schmerzmedizin, 3. Auflage, Springer-Verlag Berlin-Heidelberg
• Reit, W.; Helmberger, T. (2020); Rückenschmerz. Radiologe 60, 107–108 (2020). https://doi.org/10.1007/s00117-019-00640-x
• Guic E, Rebolledo P, Galilea E, Robles I. Contribución de factores psicosociales a la cronicidad del dolor lumbar [Contribution of psychosocial factors in chronic low-back pain]. Rev Med Chil. 2002 Dec;130(12):1411-8. Spanish. PMID: 12611243.
• Heger, S. Zur Psychosomatik des Failed-back-Syndroms: warum Rückenschmerzen chronifizieren Plädoyer für einen zeitgemäßen Umgang mit den Lumbago-Ischialgie-Syndromen. Nervenarzt 70, 225–232 (1999). https://doi.org/10.1007/s001150050426
• Wippert, P., Wiebking, C. Stress and Alterations in the Pain Matrix: A Biopsychosocial Perspective on Back Pain and Its Prevention and Treatment. Int. J. Environ. Res. Public Health 2018, 15(4), 785; https://doi.org/10.3390/ijerph15040785
• Neustadt, K., Kaiser, U., Sabatowski, R., 2017/12/04 Das biopsychosoziale Schmerzmodell: Leidfaden Heft 2017 Heft 4 10.13109/9783666402906.49
